
Welcoming AI and RPA – Healthcare’s New Automated Approach

Table of Contents
While change might be scary for some, it is, often, necessary for survival. This has never been truer than in the world of healthcare, especially in the back office processes. And RCM organizations are adopting RPA and AI as part of their transformation to becoming efficient facets of the healthcare system.
Talk to Our Automation Expert!
+91 855-975-9735
Want to experience Intelligent Automation in Action or Need help Building the Right Automation Plan?
AI applications in RCM are still in their early stages. However, as this technology advances, the possibilities for its application in RCM become increasingly limitless. Finally, the more tasks that can be automated, the better for RCM businesses, staff, and patients. Employees can be freed from boring activities and focus on those that require a human touch, such as communicating with and reaching out to patients.
RPA with AI at its Next Level in Healthcare
Given that AI is essentially a brain and RPA is essentially the hands, what if the "brain" and the "hands" were combined and applied to RCM processes? AI may perform the required "thinking" and then instruct RPA to complete the work. In a nutshell, the artificial brain (AI) makes decisions that activate the hands (RPA).
Some of the RCM processes where the combination of AI and RPA can be effective include:
- Patient registration and eligibility verification
- Appointment scheduling
- Claims processing
- Coding and documentation assistance
- Payment posting and reconciliation
- Patient billing and invoicing
- Pre-authorization and pre-certification
- Follow-up and collections
- Data analytics and reporting
- Contract management
- Compliance monitoring
- Refund processing
Know the Good Fits to Automate Healthcare
Healthcare RCM with its numerous rule-based processes, deem to be a good fit for RPA.
Candidate processes for RPA implementation are:
- Capturing patient demographic details into practice management software like Centricity, Kareo, etc.
- Verifying the procedures performed (CPT or HCPCS codes) and diagnosis codes (ICD-10 codes)
- Entering charge capture information
- Checking the status of submitted claims
- Generating patient billing statements including Explanations of Benefits (EOBs) where applicable
- Verifying claims before submission
Robotic Process Automation (RPA) and AI can enhance the speed, performance, and accuracy of billing processes. It can help overcome bottlenecks in the Revenue Cycle Management (RCM) workflow, reduce overall operational costs, and provide further benefits.
AI combined with RPA creates a virtual workforce that collaborates with humans in the RCM back office to:
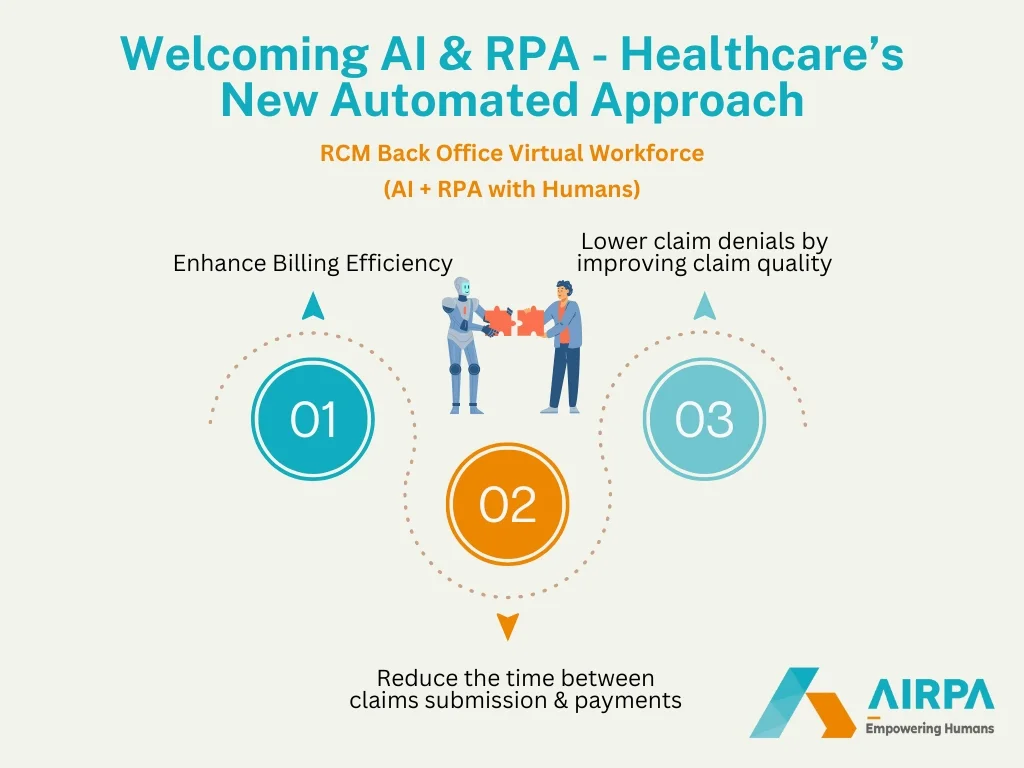
- Enhance billing efficiency
- Reduce the time between claims submission and payments
- Lower claim denials by improving claim quality
Implementing RPA would necessitate changes in technology infrastructure and process upgrades. However, these changes should not be viewed as obstacles in deploying RPA bots to streamline work and improve outcomes. The key aspect is having a clear understanding of the objectives and expected benefits of an RPA implementation, which will help in being adequately prepared with the necessary inputs.
Ask These Questions to Determine if RPA Implementation is Necessary
There is no universal approach to RPA implementation. Each organization should evaluate their unique needs, existing technologies, data, processes, and ability to drive and adopt change. As you consider implementing RPA, ask yourself the following questions to identify opportunities that are well-suited for integrating this technology:
- Can the process be broken down into a set of if/then decisions and business rules?
- Does the process require human intervention, such as critical thinking, to complete?
- Is the data accurate and accessible to RPA bots?
- How much total labor time could be eliminated or redeployed through automation in the current process?
- What impact could it have on patients? Could it increase or decrease patient satisfaction?
- Can the automated process incorporate a built-in monitoring system to mitigate risk if a step is delayed or fails? What is the risk to the business if a step fails?
- If RPA is a viable option, does it provide a complete solution, or are complementary tools required as part of the automation toolkit?
- How can the application be scaled and implemented across the organization to deliver greater value?
Final Words
As you aim to optimize your healthcare organization's business model by implementing AI & RPA for your revenue cycle, you must:
Adopt a New Mindset
Prioritize automating high-volume, simple tasks that can drive operational efficiency, enhance the customer experience, and provide employees with more engaging, higher-value roles.
Plan with Foresight
Anticipate the implications of automation on your organization's future plans, investments in digital data assets, workforce competencies and skills, and workspace planning.
Embrace a New Approach
Challenge and incentivize employees to drive tangible benefits from RPA and enhanced intelligent automation. Monitor results and prioritize future RPA initiatives based on learnings.
The role of AI and analytics in the US RCM market is significant, offering healthcare providers advantages that include increased operational efficiency and cost efficiency, reduced errors and greater patient satisfaction. Visit www.AIRPA.us to learn more about the latest in "AI & RPA healthcare solutions", which are helping enterprises harness the full potential of AI by integrating it seamlessly throughout the organization.
Popular Tags:
Related Articles

How Automation and AI are Reshaping the Fintech Landscape
Is AI the driving force behind fintech's rapid evolution?





